Tests in mice suggest the compound helps break down the cell walls of tumors, almost like destroying a tumor cell’s “skeleton”.
The researchers will test the new compound for safety and hope they can develop it to treat cancers such as colon cancer, esophageal cancer, liver and skin cancers.
“I was using these cancer cells as models of the normal intestine,” Schaefer said in a telephone interview.
Normal human cells are difficult to grow and study in the lab, because they tend to die. But cancer cells live much longer and are harder to kill, so scientists often use them.
Schaefer was looking for drugs to treat the inflammation seen in Crohn’s disease and ulcerative colitis, both of which cause pain and diarrhea. She was testing a compound called a PPAR-gamma modulator. It would never normally have been thought of as a cancer drug, or in fact a drug of any kind.
“I made a calculation error and used a lot more than I should have. And my cells died,” Schaefer said. A colleague overheard her complaining.
“The co-author on my paper said,’ Did I hear you say you killed some cancer?’ I said ‘Oh’, and took a closer look.”
They ran several tests and found the compound killed “pretty much every epithelial tumor cell lines we have seen,” Schaefer said.
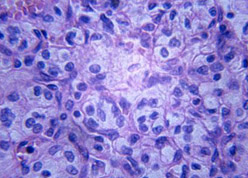
Epithelial cells line organs such as the colon, and also make up skin.
It also killed colon tumors in mice without making the mice sick, they reported in the journal International Cancer Research. The compound works in much the same way as the taxane drugs, including Taxol, which were originally derived from Pacific yew trees.
“It targets part of the cell cytoskeleton called tubulin,” Schaefer said. Tubulin is used to build microtubules, which in turn make up the cell’s structure.
Destroying it kills the cell, but cancer cells eventually evolve mechanisms to pump out the drugs that do this, a problem called resistance.
“Resistance to anti-tubulin therapies is a huge problem in many cancers. We see this as another way to get to the tubulin,” Schaefer said.
The PPAR-gamma compound does this in a different way from the taxanes, which might mean it could overcome the resistance that tumor cells often develop to chemotherapy.
“Most of the drugs like Taxol affect the ability of tubulin to forms into microtubules. This doesn’t do that – it causes the tubulin itself to disappear. We do not know why.” Schaefer’s team plans more safety tests in mice.
As the compound is already patented, her team will probably have to design something slightly different to be able to patent it as a new drug.
