The most rapid progress in the field of healthcare is in terms of technology. From X-rays to CT scans and from elaborate testing apparatus to sleek diagnostic kits, healthcare technology is progressing faster than doctors can catch up and the general public can comprehend.
All innovation; off course arises from need. And the need has always been the basic reduction of mortality and morbidity. Although at the cutting edge of technology are innovations like the complete artificial heart, the first logical step in combating any illness is early and correct diagnosis.
Misleading or false diagnosis can cost a patient’s life. Subtle differences in the countless variations in disease conditions imply different prescription of medication and different treatment. To add to the confusion, there is patient history and contraindications to consider.
Although there is no substitute for a physician’s experience and judgment, modern technology is aiding in ways no experience can substitute for.
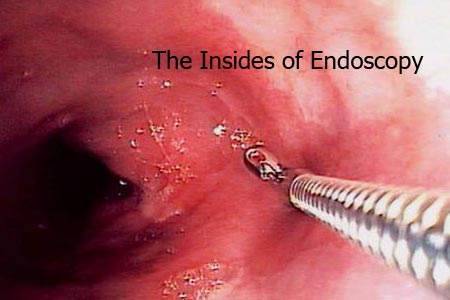
Which brings us to our topic, endoscopy or more commonly, guided surgery. Endoscopy means looking inside the body. It involves inserting of probes inside the body through normal bodily orifices or through small incisions which enable the physician to visualize the area in question better and facilitate diagnosis.
The system consists of a trocar or cannula through which is passed:
The camera gives an output on a TV screen based on which the surgeon operates. The basic premise of making the diseased area as visible as external surfaces is applicable to all specialties and hence endoscopy finds applications in different forms in almost all specialties.
It is most commonly used in:
In some cases, a small incision is made in cases such as Laproscopy Arthroscopy. While on the field in Miraj, I had the opportunity of witnessing some of these surgeries at Ashvini Prasad Hospital.
Minimum Invasive /Keyhole surgery: These are in most cases, operative procedures. For diagnostic purposes, Sonography, X-ray and other methods are first tried. If these are inconclusive, then an exploratory endoscopy may be performed which may turn into an operation. The indication, therefore, is undiagnosed chronic pain of unknown origin.
Cholecystectomy: or removal of gall bladder is one of the oldest and most common procedures performed by laproscopy.
Typically, 3-4 incisions of 5-10 mm are made, where one just below the navel for the camera. Second on the sides for the surgeons hand instruments and one above for irrigation and other instruments.
Hence the name; ‘Key-hole surgeries’. Traditional open surgeries may take less time but can require up to 20 cm cuts which greatly increases post-operative pain, risk of infection and recovery period.
Arthroscopy: It is endoscopy performed for diagnosis or treatment of joint pain. A camera and instruments are introduced through small incisions over the joint. This is most commonly performed in case of sports injuries. It is therefore, an elective surgery.
Infertility treatment: This treatment by way of endoscopy is fast catching on. Infertility can be due to a variety of causes and many different modes of treatment may be elicited from counseling to medication. However, endoscopy is proving to be a great tool in diagnostic and therapeutic gynaec cases and in assisted reproduction.
Other procedures include bronchioscpies (lungs), gastroscopies (upper GI tract), colonoscopies (lower GI tract) etc.
What does it mean to me?
Understand the pros and cons:
The cost of a laproscopic procedure still remains up to 20% higher than open surgery. A routine cholesystectomy or hernia performed laproscopically can cost anywhere between 10 to 25 thousand in a nursing home with basic amenities. In a premium hospital the cost can go upwards towards 50 thousand depending on the type of bed. The cost differential is wider in Metros. However, lesser hospitalization time and lesser chances of post-operative complications such as infections; when taken in to account, the difference in cost may not be so high. Even for a hospital, especially in big cities, lesser hospitalization time means faster turnover of patients and more business. However, 1-3 days of observation might still be needed.
Despite seeming like the best choice, a guided procedure may not always be the best option. A surgeon has to consider the merits of each case before deciding. Patient and family counseling is therefore, very important.
One should know, at least the very basics:
Advantages:
Drawbacks:
Know the surgeons credentials:
In India, there is no standardized training programme as yet. In some specialities such as ENT, Gastroenterology and Urology, guided procedures are very much a part of the post graduate curriculum. But in case of other specialties and institutes that don’t have the required facilities, a surgeon would have to acquire these skills practicing for years with other surgeons before he or she has the necessary knowledge and confidence to head such a procedure.
Although workshops and other programmes which are mushrooming every where do provide training, a universal standard and certification is lacking. Hence, no special documentation is required of a surgeon to perform such procedures. This coupled with the increasing availability of equipment in all grades of quality to whoever is willing to pay and the increasing competition in medical practice can entice many an aspiring surgeons to set up services without the adequate set-up or skill level.
So, always ask if a minimal invasive procedure is possible and feasible. Remember always to get a second opinion. Meeting a few other doctors would help, especially in case of a planned surgery. And as always, health insurance would make the decision easier and facilitate the most comprehensive treatment.
The State of Technology:
Although development of modern endoscopic techniques started more than a century back, it has been perfected and become common practice in India only in the last two decades. Of course; like any new technique, it is more prevalent in Metros. However, it is catching on in the interiors.
Take for example, Islampur: a taluka of Sangli, 30 kms from the district headquarters. I met a surgeon, Dr. Ravi Yadav, who operates the only video endoscopic unit in the taluka with a resident population of about 1 lakh and a population of 4 lakh in the surrounding villages. About 8 years ago, Dr. Yadav’s father passed away due to a case of GI bleeding which could not be diagnosed as there was no endoscopy unit till the next city, Sangli.
Disposable trocars are required for endoscopic procedures. A good one costs over Rs. 1000. The cost of a single routine diagnostic procedure; therefore, would be more than a thousand rupees. Dr. Yadav, who was kind enough to show me around the endoscopic room and explain to me some of the intricacies, maintains the set-up not for the practice it generates but for emergency cases. A case of GI bleeding can thus be diagnosed readily. The 1 hour it would take to rush the patient to the nearest city can be fatally crucial.
In addition to the infrastructure required, operating under image guidance involves a steep learning curve. In contrast, technology continues to progress by leaps and bounds. While most centers in India are yet to upgrade to a 3-chip camera from a single chip one (for better picture definition), technology involved in what is called capsule endoscopy is already being refined.
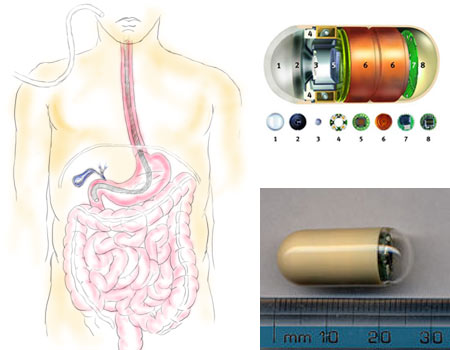
Traditional GI endoscopy involves inserting a flexible scope down the food pipe or up the colon. This procedure, despite its good reach and results and accompanying discomfort to the patient cannot satisfactorily diagnose cases of small intestine.
This is where capsule endoscopy comes in. a probe which is almost indistinguishable from a normal capsule at about 2 cm length and less than 1 cm diameter has to be swallowed. That’s it. The capsule contains a light source, a chip camera that clicks two images every second, a battery and a transmitter that transmits the images to an externally worn device. It is to be swallowed like any other pill and like food, it would travel the entire length of the stomach in roughly 12 hours (it is disposable). It can thus thoroughly survey areas that were impossible to reach non-operatively.
While still in nascent stages, the technology is available in India for critical cases. But at over 20,000, this may be the most expensive pill you ever pop!
-Punit G. Pania
Special thanks:
Dr. Sishir Gosavi, MS, DORL,
Ashvini Prasad Hospital and Post Graduate Institute,
Miraj, Sangli.
and
Dr. Ravi Yadav, MS
Shree Surgical Hospital and Hand Trauma Clinic,
Islampur, Sangli.