However, the search for alternatives to embryonic stem cells seems to have led to few hopeful yet difficult approaches. For instance, some appear to engage spermatagonial stem cells (SSCs).
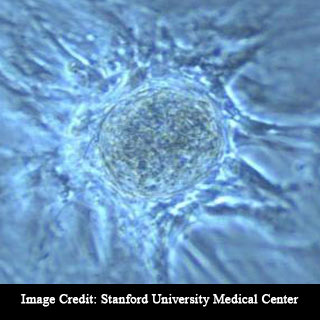
In recent times, researchers observed for example that SSCs which are developed in the laboratory may ultimately increase to a few cells. Supposedly, these cells look and act like embryonic stem cells. Though, this process could require months, only a small percentage of the SSCs may be converted into ‘embryonic stem-like’ cells.
Other researchers were believed to have used viruses in order to insert genes into SSCs which would stimulate them to turn into ES-like cells. But this approach seems to be difficult. Also, the use of viruses to transfer in the needed genes seems to have caused concern.
The latest method was noted to take the benefit of the remarkable interaction between two types of tissue namely the epithelium and the mesenchyme. The epithelium was known to line the cavities and surfaces of glands and various organs. In addition, it secretes enzymes and other factors which appear to be vital in carrying out the function of these tissues. The mesenchyme is recognized as the connective tissue located in the embryos. In adults, the connective tissue is called as stroma.
During the 1950s, scientists discovered that the epithelium seems to obtain its developmental instructions from the mesenchyme. For instance, when researchers placed bladder epithelial cells on the mesenchyme of a prostate gland, they observed that the bladder cells seemed to have changed into prostatic epithelium. Thus, the prostatic mesenchyme supposedly, changed the outcome of the bladder epithelium.
“The mesenchyme – it’s the director; it’s controlling the show,†says lead researcher and University of Illinois veterinary biosciences professor Paul Cooke.
Allegedly, Cooke began the effort with what he thought as an improbable plan.
He further stated that, “Could we take spermatagonial stem cells and cause them to directly change into other cell types by putting them with various mesenchymes and growing them in the body? I thought it was possible, but I didn’t think it would work.â€
In order to perform the research, Postdoctoral researcher Liz Simon placed SSCs from inbred mice on prostate mesenchyme and attached the combination into living mice. The findings revealed that the SSCs seem to have become prostatic epithelium. In addition, when the SSCs were combined with skin mesenchyme and grown in vivo, the SSCs appear to have become skin epithelium. Evidently, the researchers were also able to convert SSCs into uterine epithelium with the assistance of uterine mesenchyme.
Cooke elucidated that the findings revealed that the newly formed tissues seem to have all the physical characteristics of prostate, skin or uterus. Also, these tissues were believed to have produced the telltale indicators of those tissue types and they stopped looking and behaving like SSCs.
In order to confirm that their tests were not infected with epithelial cells from the source of the mesenchyme cells, the researchers repeated their experiments. They performed the experiments with the help of a mouse whose cells comprises a gene which turns green under ultraviolet light.
The researchers found that the SSCs seemed to be obtained from a green-fluorescing mouse. However the mesenchyme appears to have come from a non-fluorescing mouse. This led the researchers to draw the outcome of the SSCs. The researchers found that the newly formed prostatic epithelium seems to glow green despite the fact that the mesenchyme did not. For example, they evidently recognized that the SSCs had been converted into prostatic epithelium.
Cooke anticipates that in future, a more efficient approach might perhaps be developed which would make use of a man’s own SSCs and stroma in order to produce new skin cells or other tissues when needed. For instance, in order to replace a skin that has been damaged in a burn.
The findings of the research have been published in the journal Stem Cells.
