It was discovered that diabetics deficient in vitamin D can’t process cholesterol normally. Thus the threat of heart attack and stroke is increased as the cholesterol is supposedly built up in their blood vessels. A mechanism connecting low vitamin D levels to heart disease risk is recognized by the new research. It may lead to ways to repair the problem by increasing the levels of vitamin D.
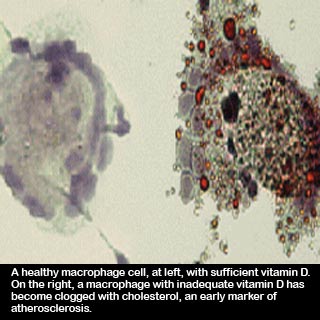
Principal investigator Carlos Bernal-Mizrachi, M.D., a Washington University endocrinologist at Barnes-Jewish Hospital commented “Vitamin D inhibits the uptake of cholesterol by cells called macrophages. When people are deficient in vitamin D, the macrophage cells eat more cholesterol, and they can’t get rid of it. The macrophages get clogged with cholesterol and become what scientists call foam cells, which are one of the earliest markers of atherosclerosis.â€
Macrophages are known to be transmitted by the immune system in response to inflammation and often seem to be stimulated by diseases such as diabetes. Bernal-Mizrachi and his colleagues are of the opinion that macrophages become full with cholesterol and ultimately stiffen blood vessels and obstruct blood flow in diabetic patients with insufficient Vitamin D.
The macrophage cells taken from people with and without diabetes and with and without vitamin D deficiency are studied by Bernal-Mizrachi, an assistant professor of medicine and of cell biology and physiology. His team led by research assistants Jisu Oh and Sherry Weng, M.D. uncovered the cells to cholesterol and to high or low vitamin D levels. Macrophages from diabetic patients were apparently more expected to become foam cells when vitamin D levels were low in the culture dish.
The team accounts that vitamin D supposedly controls signaling pathways connected both to uptake and to clearance of cholesterol in macrophages.
Bernal-Mizrachi explained “Cholesterol is transported through the blood attached to lipoproteins such as LDL, the ‘bad’ cholesterol. As it is stimulated by oxygen radicals in the vessel wall, LDL becomes oxidated, and macrophages eat it uncontrollably. LDL cholesterol then clogs the macrophages, and that’s how atherosclerosis begins.â€
The process goes faster when a person is lacking in vitamin D. People with type 2 diabetes are apparently very likely to have this deficiency. All over the world, apparently an estimated one billion people have inadequate vitamin D levels. Compared to the women who are of the same age and have no diabetes, women with type 2 diabetes have supposedly one third higher likelihood of low vitamin D.
Vitamin D is manufactured by the skin in response to ultra violet light exposure. But when the sun rays are weaker during winter and people stay indoors, then people in the US are not able to make enough vitamin D.
The good news is apparently when human macrophages are located in an environment with ample vitamin D, their uptake of cholesterol is concealed, and they don’t become foam cells. Bernal-Mizrachi is of the opinion that it may be possible to assist them to regain adequate vitamin D levels by slowing or reversing the development of atherosclerosis in diabetes patients.
Bernal-Mizrachi mentioned “There is debate about whether any amount of sun exposure is safe, so oral vitamin D supplements may work best. But perhaps if people were exposed to sunlight only for a few minutes at a time, that may be an option, too.
He has now commenced a new study on diabetics who are both lacking in vitamin D as well as have high blood pressure. He wants to find out if the blood flow would improve and lower the blood pressure if we replace vitamin D. For this study, Bernal-Mizrachi is enrolling patients with type 2 diabetes ages 30 to 80 who are not taking insulin to regulate their blood sugar. Apparently even study volunteers should have high blood pressure.
This research was published in the August issue of the journal Circulation.
