Can a human stem cell repair damaged hearts? Well this is what researchers from Stem Cell Institute (HSCI) at Massachusetts General Hospital (MGH) and colleagues at Harvard’s School of Engineering and Applied Sciences (SEAS) claim. The researchers were headed by HSCI Principal Faculty member Kenneth Chien, M.D., PhD. They used a mouse version of a human cardiac master stem cell to produce an operating strip of mouse heart muscle with technology which was developed by Kevin Kit Parker, the Thomas Dudley Cabot Associate Professor of Applied Science in SEAS.
The research supposedly increased the likelihood of using induced pluripotent stem cell (iPS) technology to take a skin cell from a patient with heart disease to utilize in producing muscle tissue to mend the ailing heart, thereby preventing the requirement to repress the immune system and the odds of rejection which is claimed to be a chief problem in organ transplantation.
“This is an initial step in moving beyond heart stem cell biology towards a different level – finding a rare cardiomyogenic cell from embryonic stem cells that can proliferate on its own and could potentially be therapeutic. This work moves us closer to heart stem cell therapy. The beauty of the system our team has developed relates to the almost pure population of the exact cells, ventricular heart cells, which we’re trying to replace in a damaged heart, and then expanding and assembling them into a functioning strip of pure ventricular muscle. That has not been done to my knowledge,†commented, Chien, the director of the (MGH) Cardiovascular Research Center and the Charles Addison and Elizabeth Ann Sanders Professor of Basic Science at Harvard Medical School (HMS).
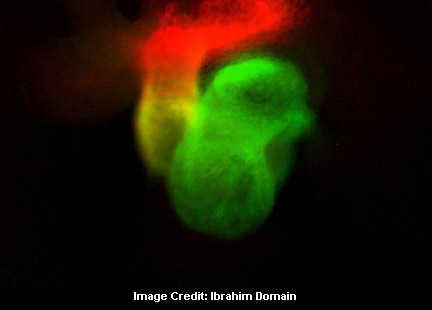
Chien added, “We’ve been able to take these very rare populations of muscle progenitors that were isolated because we were able to color code the cells. We look for the cells that have a mixed color read out. We’ve been able to take those cells and put them one layer thick on something that is almost like Saran Wrap. When they contract, they flex the film. We have the pure cells; they can be expanded, and they can make fully functional strip of muscle.â€
Packer’s lab developed the technology that generates a strip of muscle from the cardiac cells. He mentioned they try to develop technologies that are cell-agnostic; technologies that can work with Ken’s cardiac progenitors, or anyone else’s stem cells. These techniques are not limited to cardiac cells, or even to stem cells for that matter, experts claim.
Chein mentioned, “For the first time we report the identification of a cell that could be viewed as perhaps an optimal cell type to promote cardiac muscle regeneration because the cells that we use come from embryonic stem cells and then have been induced to form an intact strip of functioning ventricular muscle.â€
Chien added that the research takes the most fundamental type of undifferentiated stem cell and steers its demarcation and development to ventricular muscle and that’s the kind of muscle in the heart they are trying to regenerate.
Ibrahim Domain, commented, “What we think we have right now are the exact cell types to do this type of repair. One way or another we have to get to three dimensional muscle, which is made up of multiple layers of cells. The amazing thing about these strips we have now is that they are generating the right amount of force, but as you want to generate more force, you have to increase the thickness of the strips, and they have to have their own blood supply. There are two ways you could do this; rely on tissue engineering to produce a strip like that, or find a way to use the natural architecture of the heart to regenerate the muscle. We’re now working hard in our lab and with Kit Parker, to see how we could produce the thicker strip.â€
It is said that one might be to include the cells into a gel of some type, which could be used on the damaged muscle. Another may be to merely insert the cells into the damaged tissue, hoping that they would multiply and generate new muscle. As per Chein, fresh technology for cell delivery could be needed in either case.
Domain remarked, “In mice we’re in a position to attempt the repair right now. We can cause a heart attack, and then look for ways to repair the tissue. The simplest way is to inject the cells into the tissue – we can do that right now in mice. If that doesn’t work, we have to rely on other technologies. This is direct proof of concept that a similar approach will work with human embryonic stem cells.â€
Chein concluded by mentioning that they are in the core of the next level of challenges that face all of regenerative medicine. He thinks that they are moving quite quickly now from stem cell biology all the way through towards regenerative medicine.
The research was published in the Journal Science.