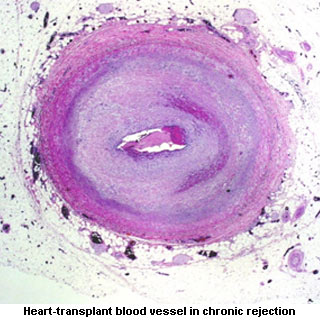
The mechanism involved in narrowing the donor’s grafted blood vessels was thoroughly analyzed. It apparently disrupts blood from reaching the transplanted organ. So due to lack of oxygen and other nutrients the organ may ultimately fail. While conducting the investigation, researchers focused the way HLA molecules on donor tissue provoke an immune response in the patient. Also how the patient’s antibodies send signals for the overgrowth of cells lining the inner blood vessels in the grafted organ was scrutinized.
“Chronic rejection is the No. 1 cause of organ failure in the first year of transplant. In the first five years, some 40 percent of organs fail after transplant due to blockage of the grafted blood vessels. Currently, we have no way to treat this deadly condition,†elucidated Elaine Reed, director of the UCLA Immunogenetics Center and professor of pathology at the David Geffen School of Medicine at UCLA.
The outcome of the research was that HLA presumably stimulated cell growth and movement depending upon a quid pro quo relationship with a molecule known as integrin beta 4. Integrin possibly allows cells to survive and spread resulting in tumor progression. Scientists predict that integrin hijacks HLA and takes over its functions. On suppressing integrin, HLA was supposedly incapable of making cells grow and migrate. Therefore, HLA is probably essential for functions of integrin like cellular movement. Further investigations will be carried out to understand the way integrin and HLA function together for boosting cancer growth.
The research will be published in the November 23 edition of Science Signaling.
